What the Inflation Reduction Act Changes
The Inflation Reduction Act was passed with a goal that many patients support: to lower prescription drug costs for people on Medicare. One of its key features is the Medicare Drug Price Negotiation Program, which gives the federal government the power to set a “Maximum Fair Price” for certain high-use medications.
These negotiated prices are intended to reduce government spending and make expensive drugs more affordable for older adults. On the surface, this seems like a win for patients. But when it comes to how drug prices work behind the scenes, the impact isn’t always what it seems.
Why This May Backfire
While drug manufacturers now must comply with these lower, government-negotiated prices, the Pharmacy Benefit Managers (PBMs) — middlemen who decide what drugs are covered and at what cost — aren’t bound by the same rules.
PBMs like CVS Caremark, Express Scripts, and Optum Rx often receive significant rebates and fees from drug manufacturers based on the original (higher) prices. When those prices are capped, the rebates shrink or disappear — cutting into PBM profits.
To compensate for that loss, PBMs may reclassify these drugs to a higher payment category, which typically means patients pay more out-of-pocket despite the drug’s “lower” price.
The result: patients face higher copays, coinsurance, or stricter coverage limits.
What the Data Showed
The study examined two anticoagulants (blood thinners)—Apixaban and Rivaroxaban—which are widely used to prevent strokes and treat blood clots. These medications are among the first affected by the IRA’s pricing program.
The modeling indicates that if PBMs move these medications to a higher coverage tier, patients might face out-of-pocket costs ranging from $ 235 million to $ 482 million more for Apixaban, and an additional $ 105 million to $ 206 million for Rivaroxaban.
The Impact on Patients
As a result, more than 320,000 patients could stop taking their medications.
Dr. Robert Popovian, Chief Science Policy Officer at the Global Healthy Living Foundation, emphasized the serious risks involved: “There are significant consequences if patients stop taking these drugs.”
This could lead to an estimated 145,000 major cardiovascular events (such as strokes or heart attacks) and up to 97,000 deaths.
“There’s direct evidence that if you stop taking your anticoagulant—and you’re a patient at risk who needs it long-term—there’s a significantly higher incidence of strokes, myocardial infarction (heart attack), and mortality. That has been well documented,” explains Dr. Popovian.
Instead of improving access to care, these pricing changes could unintentionally drive people away from life-saving treatment.
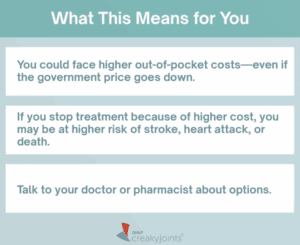
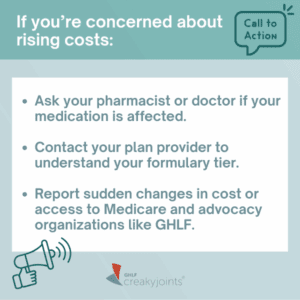
Want a quick summary of what this could mean for you?
We created an easy-to-read infographic that breaks down the paper’s key highlights — including potential cost increases, patient risks, and what actions you can take.

Lack of Transparency
One of the biggest challenges is that patients don’t see what happens behind the scenes. PBMs operate with little public accountability.
Before the IRA, Apixaban carried a high list price, often cited above $ 500, but that price was significantly offset by manufacturer rebates and other concessions paid to PBMs. With the new lower government-negotiated price under the IRA, many of those rebates may disappear—prompting PBMs to find other ways to maintain profitability, potentially by raising patient costs.
PBMs now appear to be raising patient costs directly to make up the difference. A recent report from the Pioneer Institute found that, across nine drugs affected by IRA price negotiations, average patient out-of-pocket costs increased by 32%. In some cases, costs rose by over $ 300 per prescription.
Patients may also face barriers like prior authorizations and quantity limits, making it even harder to stay on treatment.
What Policymakers—and Centers for Medicare and Medicaid Services—Must Do
While the IRA aims to reduce drug spending, it’s essential that policymakers:
- Track actual patient costs—not just the official “list price”.
- Watch for cost-shifting by PBMs that might raise patient expenses.
- Ensure transparency in rebates, fees, all concessions, all types of out-of-pocket costs, and formulary changes.
- Study the real-world impact on medication adherence and health outcomes.
Without this oversight, the system could leave behind the very people it’s meant to protect, especially seniors and those with chronic illnesses who depend on consistent access to medication.
Patients Deserve Better
Healthcare reform should never compromise access to treatment. While lowering list prices is a step in the right direction, we must ensure it does not result in higher costs and health risks for patients.
When people cannot afford the medicines they rely on, the consequences are serious—and sometimes fatal. No one should have to choose between their health and their ability to pay the bills. Patients deserve reforms that protect both their health and their wallets.
Become a 50-State Network Advocate
Joining the 50-State Network takes just a few minutes, and then you will be plugged into a nation-wide and state-by-state community of other like-minded people who are living with chronic conditions (or love someone who is). Together, we share our strength, experience, wants and needs as a patient community so that we can raise our voices with our healthcare decision-makers. Sign up today.
Healthcare Matters Podcast Interview with Robert Popovian, PharmD, MS, Chief Science Policy Officer at the Global Healthy Living Foundation.
Cools F, Johnson D, Camm AJ, et al. Risks associated with discontinuation of oral anticoagulation in newly diagnosed patients with atrial fibrillation: Results from the GARFIELD-AF Registry. J Thromb Haemost. 2021;19(9):2322-2334. doi:10.1111/ jth.15415.
Dagenais GR, Dyal L, Bosch JJ, et al. Cardiovascular consequences of discontinuing low-dose rivaroxaban in people with chronic coronary or peripheral artery disease. Heart. 2021;107(14):1130- 1137. doi:10.1136/heartjnl-2020-318758.
García Rodríguez LA, Cea Soriano L, Munk Hald S, et al. Discontinuation of oral anticoagulation in atrial fibrillation and risk of ischaemic stroke. Heart. Published online December 11, 2020. doi:10.1136/heartjnl-2020-317887.
Rivera-Caravaca JM, Roldán V, Esteve-Pastor MA, et al. Cessation of oral anticoagulation is an important risk factor for stroke and mortality in atrial fibrillation patients. Thromb Haemost. 2017;117(7):1448-1454. doi:10.1160/TH16-12-0961.
Sydor, AM, Rivera, E, Popovian, Robert. Could the Inflation Reduction Act Maximum Fair Price Hurt Patients? Journal of Health Economics and Outcomes Research. 2024 Nov 27;11(2):154-160. doi: 10.36469/001c.125251. PMID: 39629268; PMCID: PMC11612897.
The post Lower Prices, Higher Risk: How Drug Reform Could Backfire on Patients appeared first on CreakyJoints.